Unlock the Editor’s Digest for free
Roula Khalaf, Editor of the FT, selects her favourite stories in this weekly newsletter.
Scientists have recreated in a laboratory the sensory pathway that transmits feelings of pain to the human brain, in a breakthrough that could lead to better treatments.
A team at Stanford University in California is the first to combine different neurons grown from human stem cells into a functioning brain circuit in a lab dish. Their experiments, published in Nature on Wednesday, illustrate scientists’ rapid progress in replicating living tissues and organs through synthetic biology.
When the Stanford scientists exposed the brain circuit they had created to sensory stimulants, they observed waves of electrical activity travelling along it. The molecule that makes chilli peppers hot, capsaicin, immediately induced a strong response.
Sergiu Pașca, the project leader, said he expected the research to accelerate progress in understanding how the human nervous system processes pain signals.
“Now that we can model this pathway non-invasively, without using animals, we hope to find better therapeutics for chronic pain,” he said. “The best drugs we have now are opioids, derived originally from poppy seeds thousands of years ago and highly addictive.”
The researchers began by transforming skin cells into stem cells capable of generating almost any human tissue or organ. They then used chemical signals to make the stem cells form four types of “organoid” — tiny living balls representing the different regions of the pain pathway, from sensory neurons on the skin to cortical neurons in the brain.
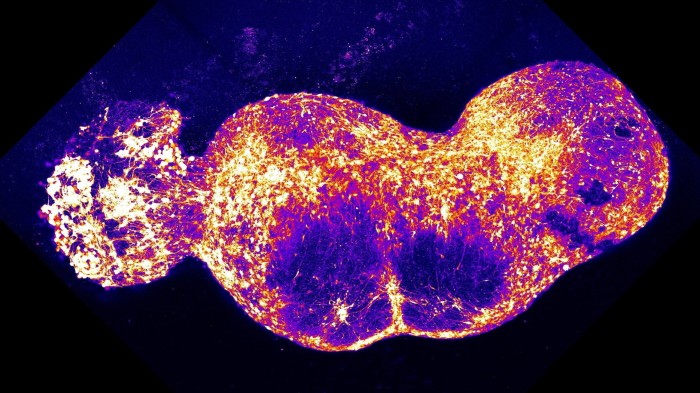
Finally the four different organoids were lined up side by side in a culture dish. After about 100 days they grew together into a synthetic representation of a brain circuit called an “assembloid”, almost 1cm long with 4mn cells. Neural connections linked the component organoids and patterns of synchronised signalling emerged.
“You would never have been able to see this wavelike synchrony if you couldn’t watch all four organoids connected, simultaneously,” said Pașca. “The brain is more than the sum of its parts.”
The assembloids themselves cannot be said to “feel pain”, he emphasised: “They transmit nervous signals that are processed by a second pathway going deeper into the brain and giving us the aversive, emotional component of pain.”
Even so, Pașca acknowledged the need to consider the ethical implications of organoid research as more complex brain circuits are created in the lab: “We are thinking very carefully about how this work proceeds, in the face of the immense need to understand psychiatric disorders and the risk of building something closer to a human brain.”
Guo-li Ming, professor of neuroscience and psychiatry at the University of Pennsylvania — who was not involved in the Stanford project — praised it for giving insights into the complexities of human neural circuitry that cannot be modelled with animals, and into how these human features lead to neurological disorders.
“This model provides the opportunity to study the complex neural network activity linking sensory input to the cortex, which was previously not feasible,” she said.
Stanford has applied for a patent on the assembloid research but has not yet decided how to commercialise it.